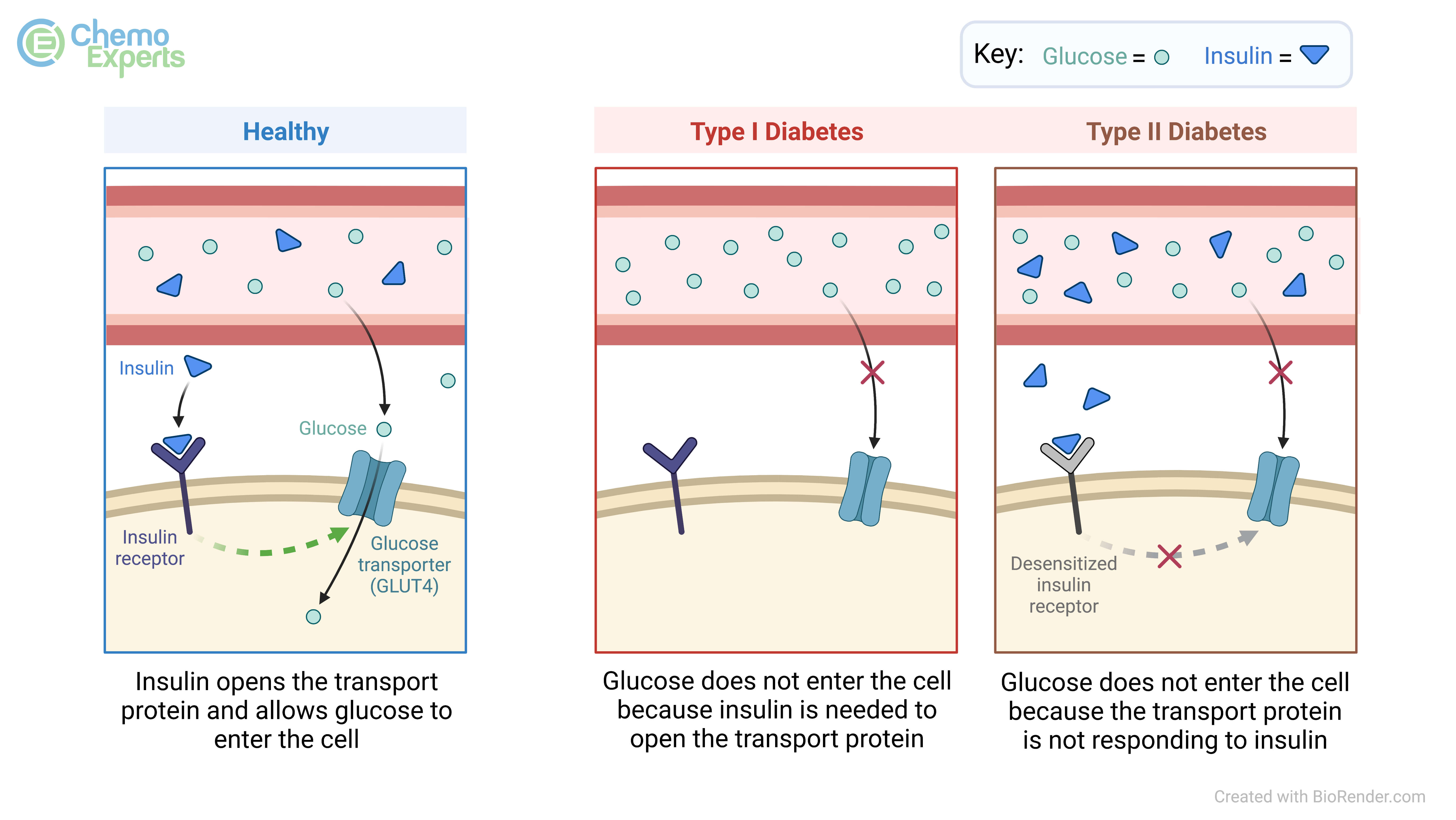
The term hyperglycemia is a medical term which means elevated blood sugars (blood glucose). This happens when the human body lacks enough insulin (type 1 diabetes), or the body cannot use insulin properly to move glucose from the bloodstream into the body’s cells (type 2 diabetes). As the human body digests the food we eat, those nutrients get absorbed from the gastrointestinal tract into the bloodstream and the glucose molecules that result need to get into the right cells to be utilized as fuel. When there is not insulin around to allow the glucose to go from the blood into the cells, this is when high blood sugars result as the glucose stays trapped in the bloodstream.
The blood sugar number is determined from either a point-of-care blood “finger prick” test using a glucometer and test strips or can be measured when a patient gets blood drawn from a vein for various other tests as well. Depending on what laboratory is running the test, and when the blood is drawn relative to the person’s last meal, the number may be low or high when compared to the normal range of values that are expected. For example, a normal fasting blood sugar (pre-meal overnight fast) range is typically any value less than 100 mg/dL based on the guidelines from the American Diabetes Association. If this value falls within the range of 100 to 125 mg/dL, this indicates you have prediabetes, and 126 mg/dL or higher indicates you have type 2 diabetes.
When a patient has consistently high blood sugars, they can experience a number of different side-effects including but not limited to frequent urination, headache, vomiting, feeling extremely fatigued or tired doing simple tasks of daily living, increased sense of being thirsty, or even blurred vision. If hyperglycemia occurs consistently and goes untreated, the result is blood vessel, nervous system, and end organ damage. Depending on the organs that get damages, the end-result of untreated high blood sugars can be heart problems (heart attacks, stroke) or nervous system problems (poor eyesight or loss of feeling in hands and feet), and poor circulation (poor wound healing).
There are many risk factors that put patients at risk for experiencing hyperglycemia. Many risk factors are associated with those who are predisposed for diabetes and include:
- Family history of type 1 or 2 diabetes
- Being of African American, Native American, Hispanic or Asian American descent
- Being overweight as defined by a BMI > 25
- Consistently high cholesterol
- Consistently high blood pressure
- History of polycystic ovarian syndrome (PCOS) or gestational diabetes
Beyond these known risk factors in patients who are predisposed for either type of diabetes, there are other risk factors for hyperglycemia in non-diabetic patients, such as those undergoing treatment for cancer. These include but are not limited to:
- Physical stress (due to illness or treatment-related infection)
- Emotional stress (due to depression, anxiety or extreme distress surrounding the diagnosis)
- Taking corticosteroids as part of the treatment regimen
- Certain chemotherapy medications such as alpelisib (Piqray®), copanlisib (Aliqopa®), everolimus (Afinitor®), brigatinib (Alunbrig®), and L-asparaginase (Erwinia®, Oncaspar®, Rylaze®)
- Being less active than usual due to cancer treatments
- Invasive surgery or physical trauma due to aggressive disease
- As a direct result of pancreatic insult secondary to treatment toxicities
It should also be noted that diabetic patients who struggle to manage hyperglycemia are at an increased risk of developing certain cancers, mainly solid tumors (breast, liver, bladder, and pancreatic to name a few). A hyperglycemic state can lead to unwanted proliferation, invasion and migration, and prevention of cancer cell death; this is an ongoing area of research.
One of the most effective ways to help prevent hyperglycemia is to follow a good healthy diet. Diets that focus on whole grains, legumes, nuts, fruits, and vegetables and those that limit the amount of food that’s processed or is high in refined sugar are associated with lower risk of hyperglycemia and diabetes.
Physical activity is another way to reduce risk of hyperglycemia. As little as 150 minutes per week of exercise can lower your risk of hyperglycemia by improving insulin sensitivity and reduce fat. Exercise does not have to be strenuous. Moderate intensity activity such as a brisk walk is enough to see these benefits.
Metformin
Metformin is an oral medication that is commonly prescribed for hyperglycemia. It works by lowering the amount of glucose that is absorbed and increases the amount of glucose that moves into cells of the body from the blood stream. Metformin can cause diarrhea and other stomach symptoms when started so typically it is started at a low dose and increased over time.
Sulfonylureas: Glipizide (Glucotrol®), Glyburide (Glynase®), Glimepiride (Amaryl®)
This class of oral medications work by increasing the amount of insulin that is made in your body and makes insulin work more efficiently. It works even when blood glucose levels are low so its important not to skip meals while taking these medications.
Pioglitazone (Actos®)
Pioglitizone increases the effectiveness of insulin that is naturally made by your body. Since it only works when insulin is present, it has a lower risk of causing too low blood sugar. It has been associated with increase risk of heart failure so its not recommended for patients with a history of heart failure.
Glucagon-like Peptide-1 (GLP-1) Receptor Agonists: Dulaglutide (Trulicity®), Exenatide (Bydureon®, Byetta®), Liraglutide (Victoza®), Lixisenatide (Adlyxin®), Semaglutide (Ozempic®, Rybelsus®)
This class of medications are generally administered as subcutaneous (under the skin) injections, except for semaglutide which can be given by mouth. They work by increasing insulin when blood sugar rises, decreases hormones that cause an increase in glucose production by the liver, and slows the time it takes for food to move from the stomach to the intestines. Unlike most medications to control blood sugar, this class of medications can lead to weight loss instead of weight gain. Stomach issues such as nausea/vomiting and diarrhea are common.
SGLT2 Inhibitors: Canagliflozin (Invokana®), Dapagliflozin (Farxiga®), Empagliflozin (Jardiance®), Ertugliflozin (Steglatro®)
These oral medications work by stopping the kidneys from reabsorbing glucose into the blood stream, causing the glucose to leave the body through urination. These medications are generally well tolerated and can help with weight loss. Some risks include increased risk of urinary tract infections and bone fractures.
DPP-4 Inhibitors: Sitagliptin (Januvia®), Saxagliptin (Onglyza®), Linagliptin (Trajenta®), Alogliptin (Nesina®)
These medications are given by mouth and increase levels of certain hormones that increase the production of insulin and decreasing levels of hormones that cause more glucose to be made by the liver. These are well tolerated medications although some patients can have issues with joint and muscle pains.
Rapid-Acting Insulin: Insulin Aspart (Novolog®), Insulin Glulisine (Apidra®), Insulin Lispro (Humalog®)
These types of injectable insulin products enter the blood stream and work right away. They are typically given with meals or at certain times of the day after your blood sugar is checked (sliding scale).
Long-Acting Insulin: Insulin Glargine (Lantus®, Semglee®, Toujeo®), Insulin Degludec (Tresiba®), Insulin Detemir (Levemir®), Insulin NPH (Humulin®, Novolin®)
Long-acting insulins are given to provide your body with a higher baseline amount of insulin throughout the day so less rapid-acting insulin is needed. They are typically given at a fixed dose at the same time each day.
 +
+
 +
+