Pericarditis is defined as either 1) acute, 2) incessant, 3) recurrent or 4) chronic depending on timing and symptoms:
1) Acute: symptoms last for less than 4-6 weeks
2) Incessant: symptoms last for more than 4-6 weeks without a break in symptoms
3) Recurrent: new symptoms occur after being symptom free for 4-6 weeks
4) Chronic: pericarditis lasting for more than 3 months
The most common symptom of pericarditis is sharp, dull, or throbbing chest pain that comes on quickly. Sometimes, this chest pain can happen with breathing, coughing, and hiccupping.
If your doctor is concerned that you have pericarditis, they may have you do heart tests such as an electrocardiogram (ECG or EKG) to look at the electrical activity in the heart, and an echocardiogram (ECHO) to check the structures of the heart. Your doctor may also listen to your heart through a stethoscope to listen for an extra heart sound called a “pericardial rub” that can sometimes be heard in people with pericarditis. Other tests that may be done include testing for inflammatory markers in the blood and getting a detailed picture of the heart through cardiac magnetic resonance imaging (cardiac MRI).
Unless a patient has a history of pericarditis, preventative measures are typically not taken. If a patient does have a history of pericarditis, medications to prevent recurrent pericarditis include colchicine (Colcrys®), NSAIDs, and corticosteroids such as prednisone or dexamethasone.
Medications that reduce inflammation are the main types of drugs used to treat pericarditis. These medications include:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids
- Colchicine (Colcrys®)
- Aspirin
- Interleukin-1 blockers (anakinra (Kineret®), rilonacept (Arcalyst®))
- Azathioprine (Azasan®)
- Methotrexate (Trexall®)
- Mycophenolate mofetil (CellCept®), Myfortic®))
- Intravenous immunoglobulin (IVIG)
In rare cases, it may be necessary to remove the pericardium. This is done as a surgical procedure and is called a “pericardiectomy”.
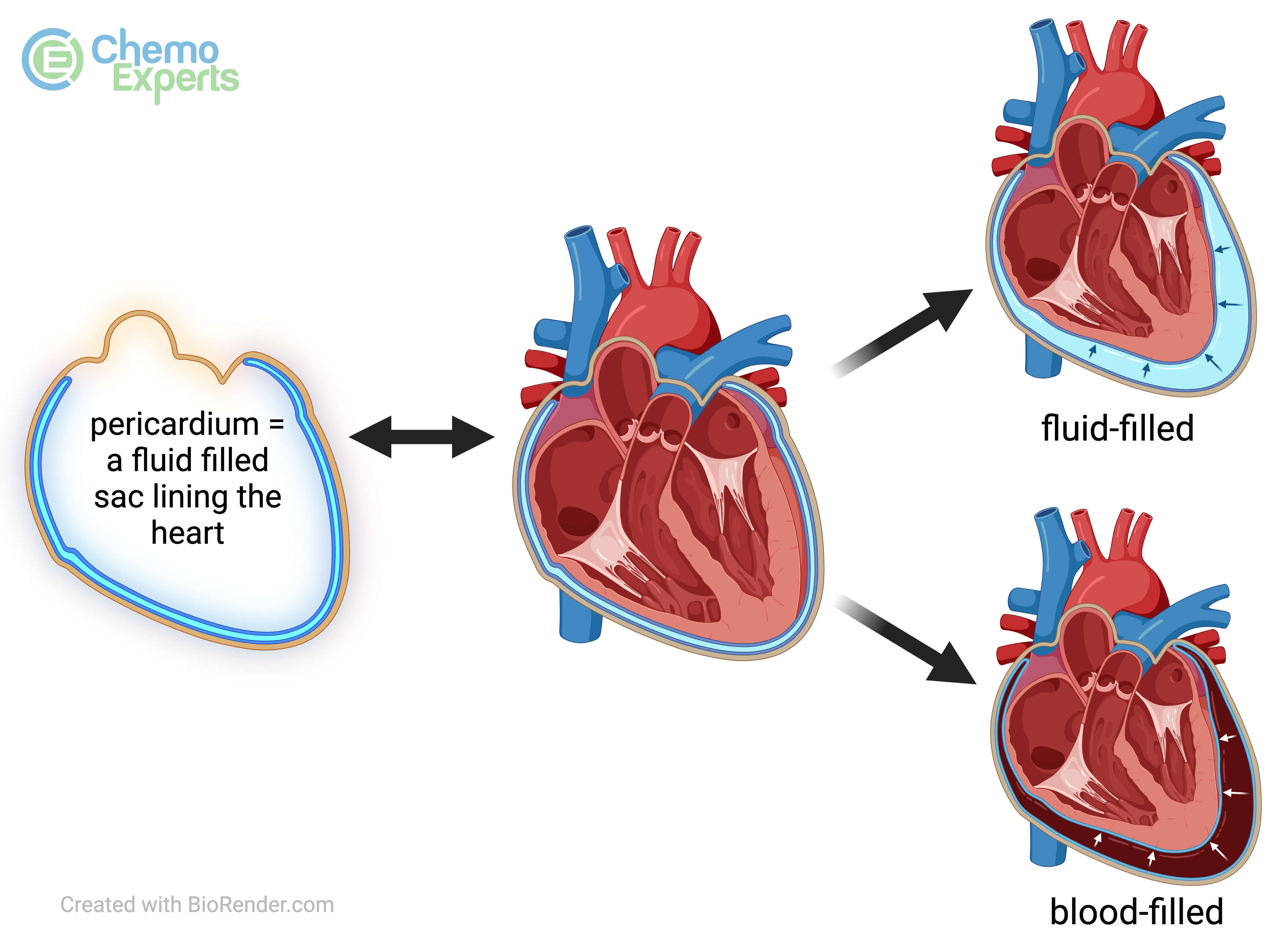
Pericarditis can sometimes cause other complications called pericardial effusions and cardiac tamponade. A pericardial effusion is a buildup of extra fluid in the pericardium, as shown below.
Cardiac tamponade is what happens when this buildup of extra fluid puts too much pressure on the heart which makes it hard for the heart to pump blood to the body. These complications require specialized treatments.
 +
+
 +
+